By Ehud Yairi, Ph.D.
University of Illinois and Tel Aviv University
Speculation on the future is a risky venture, but the accompanied excitement renders it a worthwhile one. Indeed, the outlook for stuttering research and treatment is an excitement generator. My thoughts about some future developments begin with several “facts on the ground” that will impact such a future.
Epidemiology
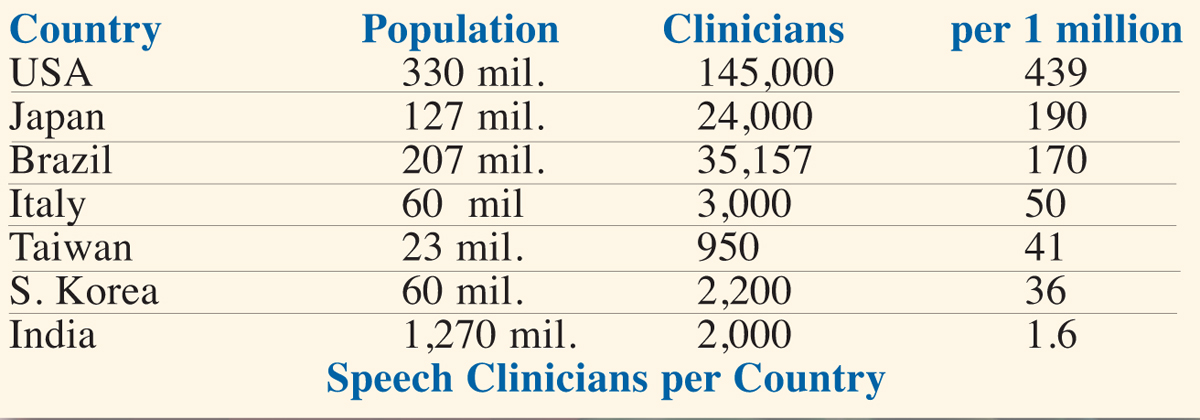
At present, 7.2 billion people inhabit our planet. Applying the conventional 5% lifetime incidence and 1% prevalence for stuttering, 360 million people world-wide have experienced stuttering in their lifetime, including 72 million exhibiting active stuttering. By 2040, the world’s population will exceed 9 billion, with 450 million people who stuttered in their lifetime and 90 million who actively stutter. Figures could be much larger if recent incidence reports of 8-11% (1; 2) are confirmed. At the same time, as seen below, professional help is limited even in advanced countries while nearly unavailable in poor ones.
The huge population with increasing economic power and growing demands, yet facing a scarcity of clinical services (most clinicians are not experts in stuttering), can be predicted to impact research toward yielding treatments with both maximal and easy reach.
Two additional facts should be considered. First, because of early stuttering onset, preschool-aged children who stutter (CWS) constitute a significant proportion of the stuttering population. Second, although most of them will experience natural recovery, some will persist. Therefore, future developments can be predicted to (a) increasingly focus on all aspects preschool CWS, and (b) discover early reliable means for recognizing risks for persistency. Note that 5% incidence-1% prevalence yield natural recovery in 4 out 5 cases, or 80%. If, however, 8% incidence is confirmed, and prevalence is only 0.7% (3), natural recovery could reach 91% (10 out of 11cases), a figure recently supported by a large UK study (5). Early identification of the 10-20% of the at-risk CWS will save much money and other resources.
Research
Genetics
Modest progress achieved during the past two decades is exciting as we and other scientists have been able to identify areas on several chromosomes where genes contributing to stuttering might be located (e.g., 4). Furthermore, a few specific candidate genes have been reported by Dr. Dennis Drayna’s NIH team (5). Stuttering now appears to involve more than just a few genes.
Future research is likely to proceed in several directions. Professor Nancy Cox, now at Vanderbilt University, has opined that the rapidly declining price-tag of genetic sequencing will allow investigators to study not only common DNA variants but also rare ones that may be unique to a single family or even a single person (6).
Biobanks will also have a major impact as medical research has been increasingly conducted through them. They present a huge advantage of allowing studies to include a wide variety of disorders. With biobanks of 100,000 already genotyped patients, it is possible to conduct association studies on many medical phenotypes at a fraction of the cost as well as time required for conventional designs (7). To speed up progress in the genetics of stuttering, speech-language clinicians must educate physicians about the importance of using the medical billing codes for speech and language disorders they recognize in patients. This will effectively provide “free” genetic data on the disorder (e.g., stuttering) and its co-morbidities. Genetic studies can be conducted successfully in data where diagnoses have been made from a combination of billing codes, physicians’ notes, pharmacy records, medical test results, etc. Because many people in biobanks have been genotyped, the data are awaiting for investigators to use them.
A major future achievement will be the uncovering of genetic elements that distinguish persistent from recovered stuttering. This endeavor began with Professor Nicoline Ambrose, University of Illinois, reporting persistency-recovery differences based on statistical genetics (8), and later by our team with Nancy Cox at the University of Chicago, employing advanced genotyping (9). Hopefully, the few active investigators of the genetics of stuttering, most notable Dr. Dennis Drayna, will also attend to this issue so critical to managing early childhood stuttering. Findings will be a major component in a clinical tool for early prediction of children in greatest need of clinical intervention.
Brain
During the past 20 years, research of brain structure and function in people who stutter (PWS) has made substantial gains. According to Professor Kate Watkin of Oxford University, findings of different studies tend to converge in regard to lo¬cations of brain differences, especially for white matter (WM); similarly so in regard to brain activities (10). She suggests that the future will see bigger studies where data can be combined across groups to study more subtle relationships among possible stuttering-related variables.
Future brain research will also increasingly target young children, with a major objective being early differentiation between the persistent and the naturally recovered subgroups. A pioneer study with 9-year-olds conducted at our Illinois program reported differences in gray and white matter between the two groups (11). Professor Soo-Eun Chang, now at the University of Michigan, has continued to lead the pursuit of this objective. Her current longitudinal study includes more than 100 preschoolers who undergo annual multimodal brain imaging for structure and function, as well as tests for behavioral variables (12).
Consequently, within a decade or so, we will be informed of structural and physiological changes that occur in the brain along the course of stuttering. For example, what is happening when children recover gradually or within weeks? At what point do abnormalities emerge (resulting in stuttering onset?) and when/how do they change across childhood? What fails to occur when stuttering persists? Is girls’ greater recovery rate reflected in greater brain plasticity? Tracking such processes will be an important element in a clinical battery for accurate risk prognosis. Furthermore, this information will be highly relevant to the question of when treatment should begin if these processes fail to occur at the expected age/time, and determining potential applications of brain stimulation, adjusted for children, as a booster to other treatments. Understanding of stuttering will also be enhanced by the new science of connectomics that seeks to build a network map of the entire physical and functional neural connections in the human brain.
Motor and Language
Evidence provided by Professor Anne Smith at Purdue University strongly suggests that from childhood to the adult years, PWS do not develop stable speech systems resistant to breakdown when demands rise. In other words, stuttering is a motor disorder. Still, she has also shown important motor/language interaction that destabilizes the motor system of PWS (13, 14). Professor Christine Weber, also at Purdue, has demonstrated that certain linguistic stimuli do elicit certain brain wave responses that differentiate CWS from NFC as well as children who persist in, from those who recover from, stuttering (15).
In my view, future research along the two paths highlighted above will generate some of the most desired information. First, scientists will be able to (a) identify neuromotor activity patterns that lead to observable stuttered speech events or are continuously present in the speech stream of PWS, and (b) identify motor patterns involved in the release from stuttered speech and back into fluency. Whereas the information will be useful in conventional speech therapy, it also might be a key element in future instrument-aided treatment discussed below. Second, there will be expanded efforts to identify brain wave responses to linguistic stimuli and early indices of speech motor development that reliably differentiate risks for persistency, thus providing a third major component to a future prognosis instrument.
Clinical Aspects
Beyond standard objectives of efficient and effective clinical services, including evaluation, counseling, and therapy, our aspirations for the future should include availability to people who stutter world-wide. With the expected 90 million people who actively stutter, current lengthy evaluations and prolonged therapeutic programs for individuals or small groups will not do.
Prognosis
As mentioned, one critical future development will be an effective tool for early identification of the 10-20% of stuttering children with highest risks for persistency. Genetics, brain structures, and brain wave data will be essential components entered into a computer program that yields accurate prognosis and is accessible by speech-language clinicians or other health personnel. We should not be surprised if the risk prognosis becomes available even prior to the child’s birth.
Treatment and Counseling
Online Distant Media
Today, nearly 40% of the world population has an internet connection. As the universe of therapies continues to adopt digital technologies (e.g., Skype), and as instrument and networking costs decline, availability of diverse live or pre-packaged therapy and counseling programs for stuttering will grow in quality while consumer audiences vastly expand. All these will be accessible to populations in regions of the world where modern clinical services for stuttering have not been available. This medium will be specifically tailored to school environments, parents, support groups, and university settings.
There will be extra benefits in elevated levels of distance services. First, outstanding stuttering clinicians, regardless of their therapeutic approach, will be conducting such long-distance therapy, making their skills benefit many more clients. Second, clinicians’ competence in stuttering therapy will be improved through distance continuing education on a much larger scale than at the present. Organizations such as the Stuttering Foundation and the International Fluency Association might assume initiatives for producing courses and therapy programs in various languages. Third, the quality of stuttering therapy in schools will be elevated through expert services. For example, a single clinician specialized in stuttering (instead of typical general school practitioners) can work simultaneously with children attending several schools. A word of caution: policies and technologies for securing privacy of certain online clinical practices must be kept in mind.
Computer Programs
Self-administered computer programs have been shown to be as effective as face-to-face therapy for treating a number of psychological disorders. Their use in stuttering therapy, however, has been limited. One example is the Kassel Program that guides clients and provide immediate feedback on voice, breathing, speed, and other variables (16). Future advances in stuttering research and in technology that enable computer programs with advance speech recognition software will not only to guide clients’ speech and other behaviors with greater specificity but also in effecting desired brain structures and physiological processes.
A few years ago, Professor Roger Ingham at the University of California called attention to this possibility in a study of the Modified Phonation Intervals computer program (17). His team reported that the level of cerebral blood flow in the putamen (a brain structure) changed towards normal for the successful group of PWS but in the opposite direction for the unsuccessful one. Cerebral blood flow correctly identified 85% of those who completed, or did not complete, the treatment. Indeed, more recent MRI imaging studies have revealed structural changes in white matter (WM) resulting from different activities, such as learning to play music, read, or juggle, often after only a few hours of training. There is also suggestive evidence that some behaviors will diminish WM (18). Keeping in mind WM deficiencies in PWS, we can expect future computer programs to fine-target such possibilities. Regardless, therapy aided by computer programs will substantially cut down direct contact hours with clinicians. Although this might be less than desirable, the advantage is that more clients will benefit from direct clinician’s attention.
Instruments
Smart devices such as cellphones will gain significant therapeutic usage, bypassing needs for specialized instruments. Auditory stimulation modes for reducing stuttering will likely increase in popularity considering that several applications are already available, including white noise, delayed auditory feedback (DAF), frequency-altered feedback (FAF), and metronomic beats. Inasmuch as Professor HeeCheong Chon, now in South Korea, or other investigators continue researching individual differences in responding to auditory feedback (19), application of this therapy mode will be significantly enhanced.
With the arrival of smaller, more sophisticated instruments, such as smart watches and biological sensors (e.g., Samsung experimental SAMI), it is not a far-fetched idea to suggest that they could be programmed for automatic speech regulation. This include speaking rate, articulatory movement within space and time, respiration, and even guide the releasing of “locked” articulatory postures. A closed-loop feedback system would deliver corrected response to undesired neural firing. Much like wireless heart pacemakers, tiny devices will record and transmit breathing and speech patterns and they will be amenable to clinicians’ long distance monitoring and control.
Biosensing devices will also be used for treating anxiety associated with stuttering. One example is the technology of virtual reality. Samsung and Google have most recently released virtual reality headsets that use smartphones as the screen. As costs decline, those rather effective instruments will be used by millions, even in poor countries.
Brain Stimulation
Advances in brain research will enhance possible applications of brain stimulation to stuttering treatment. This approach has made significant inroads in the treatment of movement disorders, such Parkinson's disease and essential tremor, as well as with depression. Very limited experiments with stuttering have included transcranial magnetic stimulation (TMS) conducted by Professor Roger Ingham (20) where a magnetic field generator is placed above the client’s head (no contact), triggering weak currents in brain regions under it. No reduction in stuttering was achieved. If updated brain data allow for more effective treatment, this method may also be considered for children. Currently, Professor Kate Watkin (21) is experimenting with transcranial direct current stimulation (tDCS), in which electrodes are positioned on the skull to send low, direct current stimulation. A third technique, deep brain stimulation, was minimally experimented with by Dr. Gerald Maguire at the University of California (22). It requires surgical implanting of electrodes deep within the brain. The electric stimulation is powered by a pacemaker-like device placed under the skin in the upper chest.
With experience being so scant, it is safer to predict that brain stimulation might be applied as a booster to other speech therapies, perhaps making progress faster and/or increase retention. Its use as a primary method will likely be reserved for the most severe, therapy-resistant cases.
Drug Treatment
Although consistent pharmacologic finding has been that medical drugs effecting lower dopamine activity (lower neuro-transmission) tend to also reduce stuttering, so far medications have not been a useful treatment option for stuttering. Side effects such as weight gain, sedation, and movement disorders are part of the problem. Nevertheless, in view of the large worldwide number of PWS, lack of clinical services, and financial constraints, effective and affordable medications are expected to become part of the therapeutic arsenal.
The large clinical study with Pagoclone that yielded some decline in stuttering was terminated. But, following experimentations with Asenapine, a new antipsychotic-dopamine antagonist drug, yielded a 60-75% drop in the stuttering of a few adults (23). The encouraging news is that Dr. Gerald Maguire and team will soon start a new study with a novel medication already cleared by the FDA for testing with stuttering.
As knowledge about genetics, brain, and motor aspects of stuttering grows, so will be the effectiveness of new medications with minimal side effects that will be discovered by a growing number of dedicated scientists. As costs decline, these medications will be available to millions, if not as a cure then as an effective aid for particular situations as needed. Intake simplicity, safety, and reliable distributers must be considered if medications for stuttering are indeed to be used world-wide. It is not unrealistic, however, to contemplate future vastly improved safe medications available over the counter. Even if not as effective as other treatments, people who stutter will be grateful to have such an aid. At present, speech clinicians should avoid recommending drugs; applications to young children are not being contemplated.
Gene Therapy
To a large extent, gene therapy is still in an experimental mode. Unlike many conventional drugs, gene therapy does not aim at treating symptoms but at correcting underlying genetic causes. The most common method is replacing a mutated gene that causes the disease with a healthy copy of same gene. Two additional methods are (a) inactivation of a disrupting mutated gene, and (b) introducing a new gene that resists the disease. The procedure can also be administered in utero, thus avoiding the disorder’s damage in early childhood. Potentially in the future, gene therapy may be capable of transforming germline cells (eggs or sperm), resulting in changes that are passed down to the next generations, that is, a permanent cure for those who inherit the gene. As per stuttering, such a scenario is not visualized for the immediate future. First, scientists must identify the specific genes underlying the disorder as well as their function. Second, the more genes are involved, the more complicated will be the challenge for therapy. We should also keep an eye on the emerging technique of optogenetics that combines genetic engineering with optics, which uses light to control the activity of genetically defined neurons. Overall, however, the venue of gene therapy as applied to humans is still a relatively a long-term future proposition.
Conclusion
Some of the future developments discussed above will probably occur faster and be more advanced than we can now even imagine. Skeptics are reminded that only one day before the first airplane flew, there was no airplane; the first flight stayed aloft for only 12 seconds, flew only 20 feet above ground, and covered a distance of only 120 feet. So is the story of many other wonderful human achievements, and so will be the story of overcoming stuttering.
References
1. Dworzynski K., Remington, A., Rijsdijk F., Howell P., & Plomin R. (2007). Genetic etiology in cases of recovered and persistent stuttering in an unselected longitudinal sample of young twins. American J Speech & Language Pathology,16,169–178.
2. Reilly S., Onslow M., Packman A., Cini E., Conway L., Ukoumunne O. Bavin E., Prior M., Eadie ., Block B, & Wake M. (2013). Natural History of Stuttering to 4 Years of Age: A Prospective Community-Based Study. Pediatrics,36, 460–467.
3. Craig A., Hancock K., Tran Y., Craig M., & Peters K. (2002). Epidemiology of stuttering in the community across the entire life span. J Speech, Language,& Hearing Research, 45, 1097–1105.
4. Suresh R., Ambrose N., Roe C., Pluzhnikov A., Wittke-Thompson J., C-Y Ng M., Cook E., Lundstrom C., Garsten M., Ezrati R., Yairi E., & Cox N. (2006). New Complexities in the Genetics of Stuttering: Significant Sex-specific Linkage Signals. American J of Human Genetics, 78, 554-563.
5. Kang C., Riazuddin S., Mundorff J., Krasnewich D., Friedman P., Mullikin J., & Drayna, D. (2010). Mutations in the lysosomal enzyme-targeting pathway and persistent stuttering. New England J of Medicine,362, 677–685.
6. Cox N. (2016). Personal communication.
7. Bowton E., Field, Wang S. Schildcrout J., Van Driest S., Delaney J., Cowan J. Weeke P., Mosley J., Wells Q., Karnes J., Shaffer C., Peterson J., Denny J., Roden D., & Pulley J. (2014). Biobanks and electronic medical records: Enabling cost-effective research. Sci Transl Med, 6 (234):234cm3. PMC4226414
8. Ambrose, N., Cox, N., & Yairi E. (1997). The genetic basis of persistent and recovered stuttering. J of Speech, Language,& Hearing Research, 40, 567-580.
9. Suresh R., Ambrose N., Roe C., Pluzhnikov A., Wittke-Thompson J., C-Y Ng M., Cook, E., Lundstrom C., Garsten M., Ezrati R., Yairi E., & Cox N. (2006). New Complexities in the Genetcs of Stuttering: Significant Sex-specific Linkage Signals. American J of Human Genetics, 78, 554-563.
10. Wattkin K. (2016). Locations reported for reduced FA in groups of people who stutter relative to controls in the white matter underlying ventral sensorimotor cortex 3D renderings of the MNI152 average brain. A personal communication.
11. Chang S., Erickson K., Ambrose N., Hasegawa-Johnson M., & Ludlow C. (2008). Brain anatomy differences in childhood stuttering. Neuroimage, 39, 1333–1344.
12. Chang S. (2015). Neural correlates of developmental stuttering: Research updates from a longitudinal study of brain development in children who stutter. Annual convention, American Speech-Language-Hearing Assn.
13. Walsh B., Mettel K., & Smith A. (2015). Speech motor planning and execution deficits in early childhood stuttering. J Neurodev Disord. 7,1-12.
14. Smith A, Goffman L, Sasisekaran, J., & Weber-Fox C. (2012). Language and motor abilities of preschool children who stutter: evidence from behavioral and kinematic indices of nonword repetition performance. J Fluency Disorders,37, 344-58.
15. Spencer C. & Weber-Fox C. (2014). Preschool speech articulation and nonword repetition abilities may help predict eventual recovery or persistence of stuttering. J Fluency Disorders, 41, 32-46.
16. Euler H. A., Wolff von Gudenberg A., Jung K., & Neumann K. (2009). Computergestützte Therapie bei Redeflussstörungen: Die langfristige Wirksamkeit der Kasseler Stottertherapie (KST) [Computer assisted therapy for fluency disorders: The long-term effectiveness of the Kassel Stuttering Therapy]. Sprache Stimme Gehör, 33, 193–201
17. Ingham R., Wang Y., Ingham, Bothe A., & Grafton S. (2013). Regional brain activity change predicts responsiveness to treatment for stuttering in adults. Brain & Language, 127, 510–519
18. Zatorre R., Fields R., & Johansen-Berg H. (2012). Plasticity in gray and white: neuroimaging changes in brain structure during learning. Nat. Neurosci. 15, 528–536.
19. Chon H., Kraft S., Zhang J., Loucks T., & Ambrose N. (2013). Individual variability in delayed auditory feedback effects on speech fluency and rate in normally fluent adults. J Speech, Language, and Hearing Research, 56,489–504.
20. Ingham R., Fox P., Ingham .J, Collins .J, & Pridgen S (2000). TMS in developmental stuttering and Tourette’s Syndrome. In: M. S. George, & R. H. Belmaker (Eds.). Transcranial magnetic stimulation (TMS). In neuropsychiatry (pp. 223– 236). New York: American Psychiatric Press.
21.https://clinicaltrials.gov/ct2/show/NCT02288598 (2016).
22. Maguire G., (2011). Asenapine for the treatment of stuttering: An analysis of three cases. Am J Psychiatry, 168, 651-652.
23. Maguire G., (2012). Alleviation of developmental stuttering following deep brain stimulation of the ventral nucleus of the thalamus. Am J Psychiatry, 169, 759
From the 2016 Summer Newsletter






 Podcast
Podcast Sign Up
Sign Up Virtual Learning
Virtual Learning Online CEUs
Online CEUs Streaming Video Library
Streaming Video Library